Charting the new era of obesity care with real-world solutions
24 Nov 2025
Share
Obesity is increasingly recognized as a multifactorial disease with deep metabolic, hormonal, and neurobehavioral roots.1 In Malaysia, its prevalence continues to rise despite growing public health efforts, a trend mirrored globally.1,2 At the symposium “The New Era of Obesity and Metabolic Syndrome Treatments: From Past Lessons to Today’s Best Practices”, Dato’ Dr. Nik Ritza Kosai Nik Mahmood, Consultant Upper Gastrointestinal and Obesity Surgeon of UKM Specialist Center, reviewed the evolution of obesity management, from foundational lifestyle interventions to the latest pharmacologic and surgical innovations. His sessions highlighted how a holistic and evidence-based approach can reshape patient outcomes in obesity and related metabolic disorders.
The growing burden of obesity
Globally, obesity has more than doubled since the 1990s, with 2.5 billion adults overweight and 890 million living with obesity in 2022.3 The condition heightens the risk of cardiovascular, respiratory, and endocrine diseases, and 13 types of cancers are more prevalent among obese individuals.3,4 “Weight reduction can halve the hazard ratio for certain cancers,” Dato’ Dr. Nik noted, underscoring that obesity is a systemic, disease-driving condition, not merely an esthetic issue. In Malaysia, the trend is equally alarming. According to the National Health and Morbidity Survey (NHMS) 2023, 54.4% of adults are overweight or obese, and abdominal obesity affects 54.5%, representing a ~20% relative increase since 2011.2
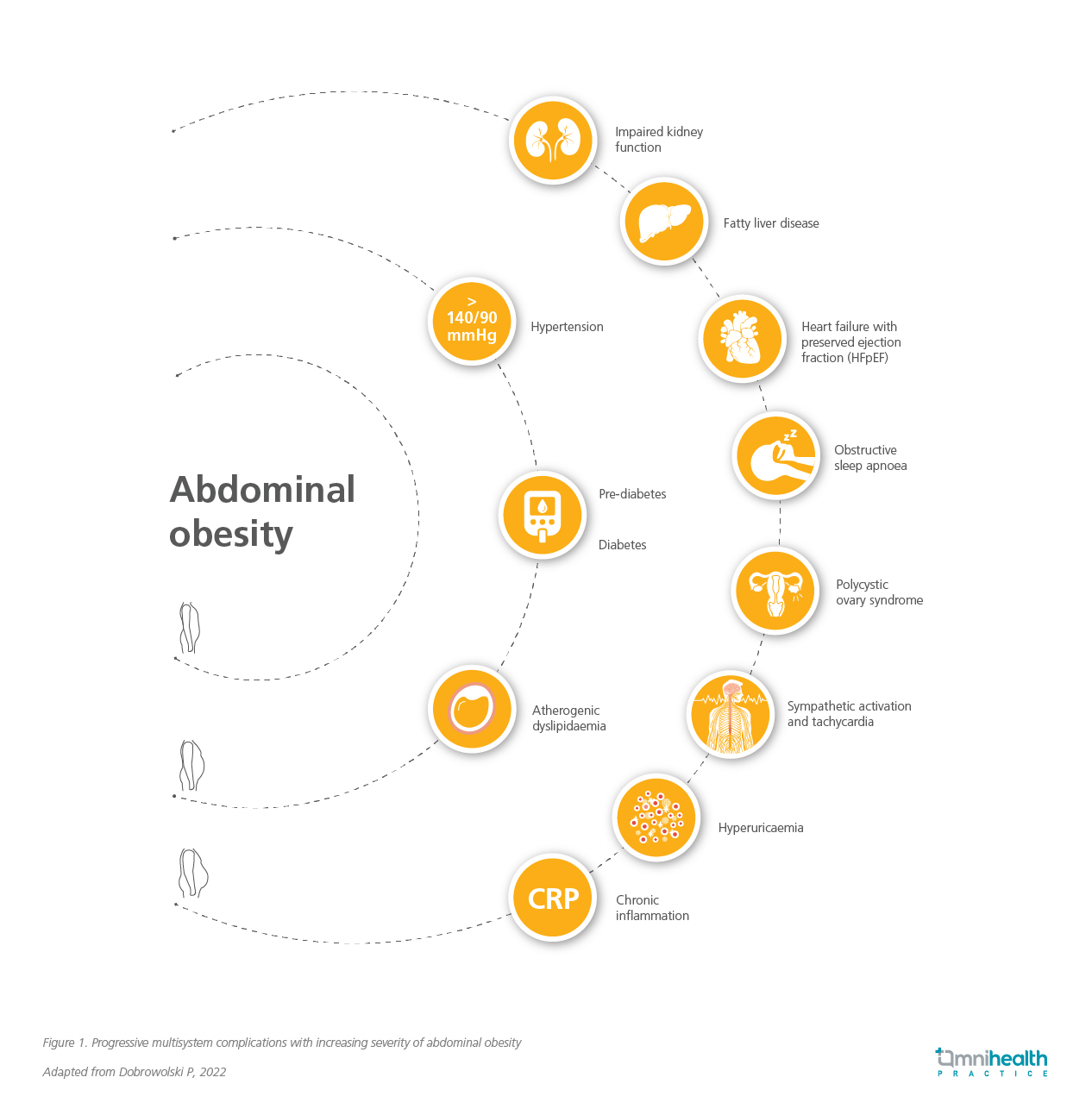
“One in two Malaysians is either overweight or obese, placing them at increased risk of metabolic complications such as type 2 diabetes,” highlighted Dato’ Dr. Nik. Beyond these numbers, abdominal obesity also drives dysfunction across multiple organ systems (figure 1).5 In “diabesity”, according to Dato’ Dr. Nik, adipocyte injury triggers inflammatory cytokines such as IL-1 and TNF-α, reduces adiponectin levels, and disrupts glucose metabolism, while long-term high-fat diets and reduced gut microbial diversity exacerbate insulin resistance, illustrating the broad systemic impact of excess adiposity.
Understanding obesity beyond calories and BMI
Obesity is a complex medical condition that extends beyond a simple energy imbalance, involving metabolic, hormonal, psychological, and genetic interactions.1,3 Body mass index (BMI) alone does not capture the full picture of obesity. Current recommendations suggest confirming excess adiposity through direct measurement of body fat or validated anthropometric criteria appropriate to age, sex, and ethnicity.4 Widely accessible, bioelectrical impedance analysis (BIA) provides an estimate of body fat composition, including fat mass, lean mass, and total body water, though it may underestimate fat percentage in overweight individuals.1 The Edmonton Obesity Staging System (EOSS) complements these measures by providing a holistic assessment of metabolic, psychological, and functional health.1
Effective obesity care requires a multidimensional approach that considers psychological health and comorbidities.1,5 “Patients with eating disorders such as bulimia or anorexia are contraindicated for bariatric surgery,” Dato’ Dr. Nik cautioned, underscoring the importance of psychological screening. In his practice, patients undergo multidisciplinary evaluation—including physiotherapy, cardiology (with computed tomography [CT] angiogram or stress echocardiogram), respiratory medicine, dietetics, and ENT (for sleep apnea screening) to establish baseline status. “Patients with obstructive sleep apnea (OSA) are placed on continuous positive airway pressure (CPAP) support for three to six months before surgery to prevent cor pulmonale,” he explained. He also noted that fatty liver disease, now the leading cause of cirrhosis and a common finding in obesity, progresses from steatosis to fibrosis and can be monitored with FibroScan. Together, these assessments underscore obesity’s systemic impact beyond glucose control.
Evolving strategies in obesity management
Obesity management now spans a continuum, from lifestyle modification to pharmacotherapy and surgery. Lifestyle changes remain foundational but yield only 5%-8% weight loss on average.6 Pharmacotherapy is the next step, offering greater efficacy but requiring individualized selection. Traditional agents include phentermine and combination therapies such as phentermine/topiramate or bupropion/naltrexone, achieving 5%-10% weight loss.6 Newer incretin-based therapies like semaglutide and tirzepatide demonstrate superior results, though local accessibility and cost remain challenges.6,7 “Every option must be weighed against cost, availability, long-term efficacy, and tolerability,” Dato’ Dr. Nik advised.
For patients not yet surgical candidates, intragastric balloons (IGBs) and endoscopic bariatric surgeries (EBS) provide effective intermediate options. Dato’ Dr. Nik explained that modern IGBs can achieve 10%-15% weight loss, while EBS yields about 20%. These options suit patients with a BMI of 27.5kg/m2-37.5kg/m2, though potential adverse effects include cramps, nausea, and gastric leak. At the apex, metabolic surgery remains the gold standard, achieving 30%-40% weight loss and durable metabolic improvements. Sleeve gastrectomy is the most common, while mini-gastric bypass (MGB) is preferred for its simplicity and reversibility. Dato’ Dr. Nik emphasized that, despite their effectiveness, the benefits of surgery must be weighed against potential risks, including bile reflux and nutritional deficiencies.
The landscape is now moving toward multimodal strategies—combining pharmacologic and procedural modalities for enhanced outcomes. Studies show that adding GLP-1 receptor agonists to endoscopic sleeve gastroplasty or IGB augments weight loss without added risk.8,9 As Dato’ Dr. Nik observed, these synergistic approaches represent a shift toward individualized, physiology-based therapy.
Conclusion
The new era of obesity care calls for integration—between specialties, modalities, and patient engagement.1,5 From past lessons to current best practices, the goal remains to enable durable, meaningful weight loss and restore metabolic health.1,5 Dato’ Dr. Nik concluded that sustainable success requires more than procedural expertise; it demands patient participation and lifestyle commitment. “The best treatment ultimately comes from patients themselves,” he reflected. As Malaysia enters this new phase of obesity care, combining pharmacologic advances, endoscopic innovation, and metabolic surgery within a team-based framework offers the most promising path toward long-term health and remission.1,5
References
- Przybyłowski A, et al. Redefining obesity: A narrative review of diagnostic evolution, therapeutic strategies and psychosocial determinants. Healthcare. 2025;13(16):1967.
- Institute for Public Health. National Health and Morbidity Survey (NHMS) 2023: Non-communicable Diseases and Healthcare Demand – Key Findings. 2024. Available at: https://iku.nih.gov.my/images/nhms2023/key-findings-nhms-2023.pdf. Accessed Oct 14, 2025.
- World Health Organization. Obesity and overweight. 2025. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed Oct 14, 2025.
- Rubino F, et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 2025;13(3):221-62.
- Dobrowolski P, et al. Metabolic syndrome—A new definition and management guidelines. Arch Med Sci. 2022;18(5):1133-1156.
- Horn DB, et al. What is clinically relevant weight loss for your patients and how can it be achieved? A narrative review. Postgrad Med. 2022;134(4):359-75.
- Aronne LJ, et al. Tirzepatide as compared with semaglutide for the treatment of obesity. N Engl J Med. 2025;393(1):26-36.
- Yilmaz A, et al. The efficacy of liraglutide combined with intragastric balloon on weight loss. Rev Assoc Med Bras. 2023;69(12):e20230571.
- Bahdi F, et al. Revisional endoscopic sleeve gastroplasty versus semaglutide and tirzepatide for weight recidivism after sleeve gastrectomy. Clin Obes. 2025;15(3):e70001.