From SABA reliance to ICS-first: Malaysia’s 2024 CPG ushers in a new era of asthma control
1 Sep 2025
Share
After an eight-year hiatus, the 2024 Clinical Practice Guidelines (CPG) for the Management of Asthma in Adults have been released, introducing evidence-based recommendations that reflect both international best practices and the unique needs of the Malaysian population.1 The long-anticipated update was presented by Associate Professor Dr. Andrea Ban Yu-Lin, senior consultant physician and pulmonologist at Hospital Canselor Tuanku Muhriz UKM, and the Chairperson of the CPG development committee, during the MTS Annual Congress 2025.1
Unlike previous editions, the 2024 CPG takes a more integrated and nuanced view of asthma management. “This is not just an update—it’s a call to action to improve asthma care,” said Dr. Andrea Ban.1 Drawing from global evidence and local consensus, the guideline prioritizes applicability across Malaysia’s diverse healthcare settings, with an emphasis on equity, accessibility, and real-world implementation.1 One of the most significant shifts in the new CPG is the clear move away from short-acting beta2-agonist (SABA) monotherapy.1 The new CPG explicitly endorse as-needed or low-dose inhaled corticosteroid (ICS)-containing regimen for initial treatment steps, in line with evidence showing that early anti-inflammatory control reduces exacerbation risk and improves long-term outcome.1
The stepwise treatment algorithm has also been restructured for greater clarity, introducing options such as Maintenance and Reliever Therapy (MART) and as needed ICS-based reliever strategies (sometimes referred to as Anti-Inflammatory Reliever [AIR]) for patients requiring controller therapy.1 These regimens simplify treatment, improve adherence, and mark a departure from the traditional fixed-dose controller plus SABA rescue model.1 Triple therapy with ICS, long-acting β2-agonists (LABA), and long-acting muscarinic antagonists (LAMA) is now explicitly outlined, with clinicians advised to reassess inhaler technique and adherence before escalating treatment.1 Consistent with a more personalized care philosophy, the guideline also provides a structured framework for the use of biologic therapies in severe asthma, supported by a locally adapted algorithm that guides selection based on phenotype, eosinophil count, and exacerbation history.1
Diagnostic criteria have been expanded to support phenotype-based treatment while maintaining spirometry as the gold standard for confirming asthma through assessment of airway obstruction variability.1 In specialized centers, fractional exhaled nitric oxide (FeNO) and blood eosinophil counts may be used to guide targeted therapy.1 In resource-limited settings, peak flow measurement remains a practical alternative, with diurnal variation calculation incorporated into the guideline as an additional method for assessing airway variability.1
To strengthen implementation, the CPG places strong emphasis on self-management and patient education.1 Patients are encouraged to follow a Personalized Asthma Action Plan (PAAP) and undergo “Teach-to-Goal” inhaler technique training, supported by adherence support and educational resources to address Malaysia’s diverse health literacy needs.1 The 2024 CPG also expands guidance for special populations, including pregnant women and individuals with occupational asthma.1 Definitions now encompass work-aggravated and irritant-induced asthma, and management recommendations extend beyond pharmacotherapy to early intervention, return-to-work planning, and psychosocial and financial support.1
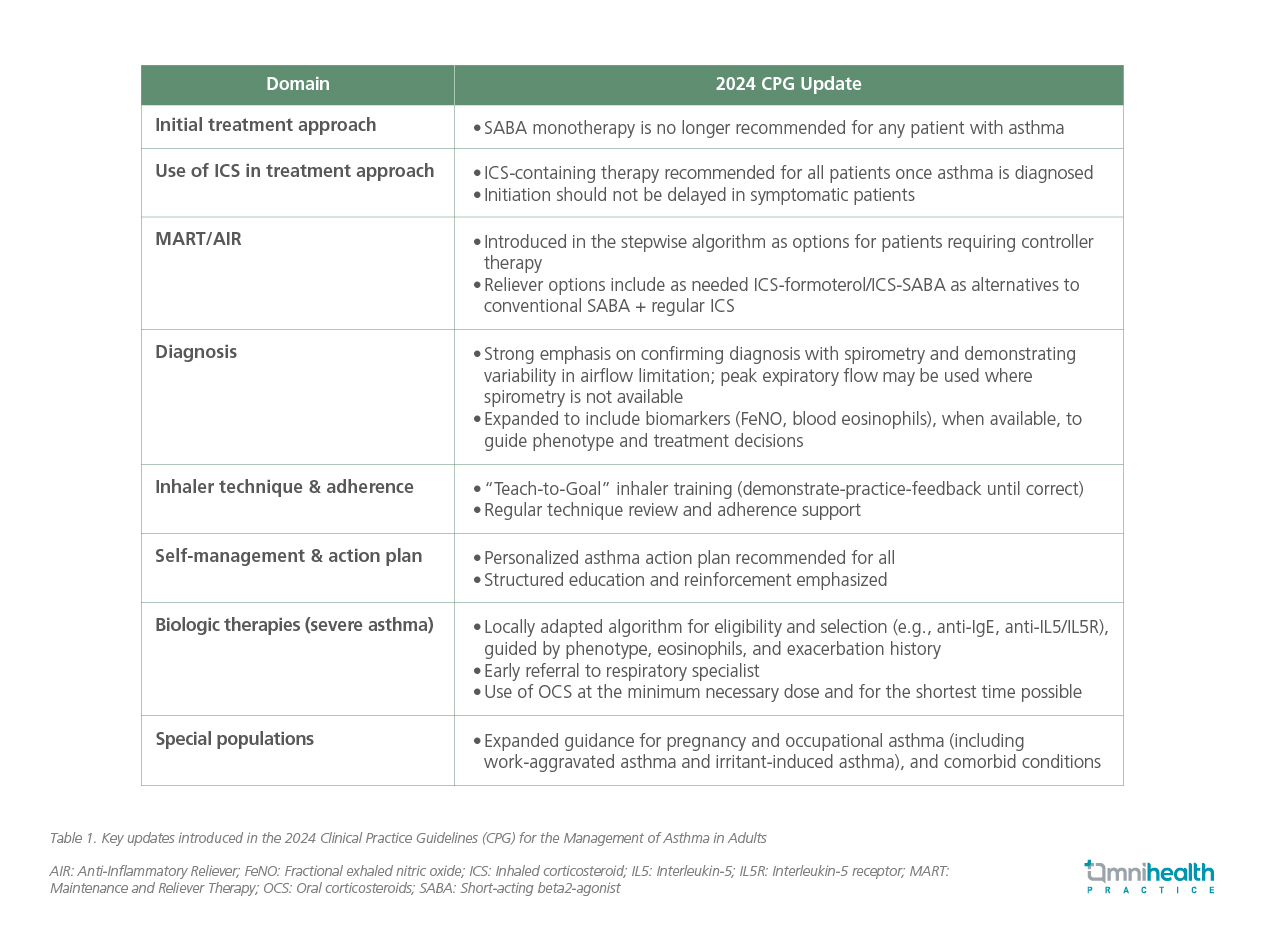
Beyond pharmaceutical treatment, the CPG highlights the need for structured multidisciplinary care, improved referral pathways, and health system integration to close the gaps in continuity of care.1 The guideline was developed through a rigorous, multidisciplinary process coordinated by the CPG Unit of Malaysian Health Technology Assessment Section (MaHTAS), Ministry of Health Malaysia, and the Malaysian Thoracic Society, ensuring alignment with the highest standards of evidence-based guideline development.1 In conclusion, the 2024 CPG is more than a clinical reference; it is a blueprint for delivering high-quality, patient-centered asthma care in Malaysia.1 Central to this vision is a clear break from SABA-only treatment, replacing it with ICS-containing regimens for all patients from the outset.1 This landmark shift, together with a stronger focus on personalized management, aims to reduce preventable asthma deaths, standardize practice, and empower both clinicians and patients toward better asthma control.1 Table 1 summarizes the key updates introduced in the 2024 guidelines.1
In an interview with Omnihealth Practice, Dr. Andrea Ban Yu-Lin reflected on the rationale behind the major updates in the 2024 CPG and the evolving landscape of personalized asthma management in Malaysia.
Q1. The new CPG emphasizes a personalized approach to asthma care. How should clinicians translate this into daily practice?
Dr. Andrea Ban: Asthma is not a one-size-fits-all disease. Management should account for each patient’s genetic predisposition, environmental exposures, and comorbid conditions. For example, a patient with elevated Type 2 (T2) inflammatory markers may benefit from targeted biologic therapy, while a non-T2 phenotype may require a different approach. The guideline also emphasizes reassessing inhaler technique, adherence, and modifiable environmental triggers before stepping up treatment.
Q2. The guideline introduces updates on diagnosis and phenotyping. Can you elaborate?
Dr. Andrea Ban: Spirometry remains the gold standard for diagnosing asthma, as it objectively confirms variable airflow limitation. Biomarkers such as fractional exhaled nitric oxide (FeNO) and blood eosinophil counts are recommended to help identify T2 inflammation and guide phenotype-based treatment decisions, particularly when considering biologics. We have also detailed the calculation of diurnal variation in the guideline, which can be useful for assessing airway variability, especially in settings where spirometry access is limited.
Q3. There are several notable updates in acute asthma management and inhaler selection. What should clinicians take away?
Dr. Andrea Ban: One key addition is the explicit inclusion of intravenous magnesium sulphate (IV MgSO4 2g over 20 minutes [single dose]) for severe and life-threatening exacerbations, incorporated with input from emergency physicians. Inhaler choice is another important area. The updated CPG outlines factors to consider, including patient’s ability to use device correctly, availability, cost, and preference. We have also adopted a “Teach-to-Goal” approach for inhaler technique training, where clinicians should provide hands-on demonstration, observe the patient’s technique, and repeat the process until correct use is consistently achieved. This structured approach is critical to achieving optimal asthma control.
References
- Ban YL. Asthma CPG revived: Key updates and advances after an 8-year hiatus. Presented at the Malaysian Thoracic Society (MTS) Annual Congress 2025; August 14-17, 2025.