“Green nephrology” turns the tide in kidney care
19 Sep 2025
Share
Climate change and environmental sustainability have become pressing concerns across healthcare, and nephrology, as one of the most resource-intensive specialties, carries a unique responsibility to act.1-3 At the 39th Malaysian Society of Nephrology (MSN) Annual Congress 2025, a plenary session on “Green Nephrology” featured Dr. Azrini Abdul Aziz, consultant nephrologist at Hospital Kuala Lumpur, and Dr. Fong Voon Ken, consultant nephrologist at Gleneagles Hospital Kuala Lumpur, who shared insights on the environmental footprint of kidney care and explored innovative approaches to advance sustainability in nephrology practice.
Going green in nephrology: A call for sustainable kidney care
Climate change is no longer a distant concern but is now recognized as a significant determinant of human health. Rising global temperatures, extreme weather events, and deteriorating air and water quality are amplifying risks for vulnerable populations worldwide.1,2 Kidney health, in particular, is directly impacted: higher ambient temperatures increase the risk of dehydration, acute kidney injury, and kidney stone formation, while flooding and natural disasters can disrupt dialysis services and access to care.4
As Dr. Azrini emphasized, the relationship is bi-directional. While kidney patients suffer from the effects of climate change, nephrology itself contributes significantly to environmental degradation.3,4 Healthcare as a whole accounts for an estimated 1%-5% of global greenhouse gas emissions, with dialysis services recognized as among the most resource-intensive.2,3 Hemodialysis (HD) and peritoneal dialysis (PD) rely on large volumes of water, electricity, and single-use plastics, generating substantial waste.2,3
The urgency of addressing sustainability in nephrology is underscored by the rising prevalence of chronic kidney disease (CKD).5 As the number of patients requiring kidney replacement therapy continues to grow worldwide, so too does the environmental burden of dialysis.5 This creates an ethical imperative: the kidney community must deliver life-saving treatments in a way that also safeguards planetary health.
Balancing patient outcomes with planetary health
The environmental footprint of dialysis is striking. According to Dr. Azrini, a standard 4-hour HD session can consume around 500 liters of water, equating to 1,500 liters per week for thrice-weekly treatments. In comparison, a conventional PD prescription (four 2-liter exchanges daily) uses about 120 liters of water per day (or 840 liters weekly) although this does not account for the hidden water cost of producing the dialysate bags.
Waste generation adds another layer of concern.6 HD is estimated to generate 2.5kg of solid waste per session (around 7.5kg weekly), with 38% comprising plastics, primarily polyvinyl chloride (PVC).3 PD generates approximately 1.8kg of waste daily (12.6kg weekly), more than half of which is also PVC.3 Beyond solid waste, dialysis consumes energy and chemicals and requires extensive packaging and transport, contributing to greenhouse emissions and carbon footprints throughout the supply chain.3
Dr. Azrini highlighted that nephrology’s mission must therefore be reframed: to maximize patient outcomes while minimizing ecological costs. Strategies such as reducing single-use plastics, introducing recyclable or biodegradable materials, improving energy efficiency in dialysis units, and integrating water-saving technologies can significantly reduce dialysis’ environmental impact.2,3,6 Importantly, sustainable care models also lower costs over time, aligning clinical, environmental, and economic goals.6
Equity at the heart of sustainable nephrology
The burden of climate change and environmental degradation falls disproportionately on marginalized populations, including children and communities with limited healthcare access.1 In Malaysia, as in many developing regions, rapid urbanization and pollution heighten these vulnerabilities.1
For kidney care, this raises a central question: can sustainability also enhance equity? Addressing this, Dr. Azrini argued that it can. Home-based PD reduces the need for hospital visits and transportation, easing patient burden while lowering environmental footprint.4 Recycling initiatives such as the locally developed “Jom Recycle” program, in which patients return empty PD dialysate bags for collection and recycling, further demonstrate how patient engagement can make dialysis more sustainable without compromising outcomes.
Despite these successes, implementing green practices in daily operations remains a challenge. Dr. Azrini explained, “Awareness is already there, but implementation is the challenge. Healthcare teams often feel that green initiatives add extra work, so continuous education and encouragement are essential to build momentum.” She further outlined practical steps for healthcare teams to translate awareness into action (table 1):
| Awareness and champions | Embedding sustainability training in healthcare staff education and appointing “eco-dialysis champions” |
| Waste triage | Separating contaminated from non-contaminated waste and recycling where safe |
| Reuse where feasible | Reusing tourniquets or bicarbonate cartridges under safe protocols |
| Energy and water efficiency | From LED lighting to solar panels and optimized water treatment |
| Sustainable infrastructure | Incorporating natural lighting and on-site waste management when building new dialysis units |
Table 1. Actionable measures to reduce the environmental footprint in nephrology
LED: Light-emitting diode
From single-pass to smart systems: Reimagining dialysis care
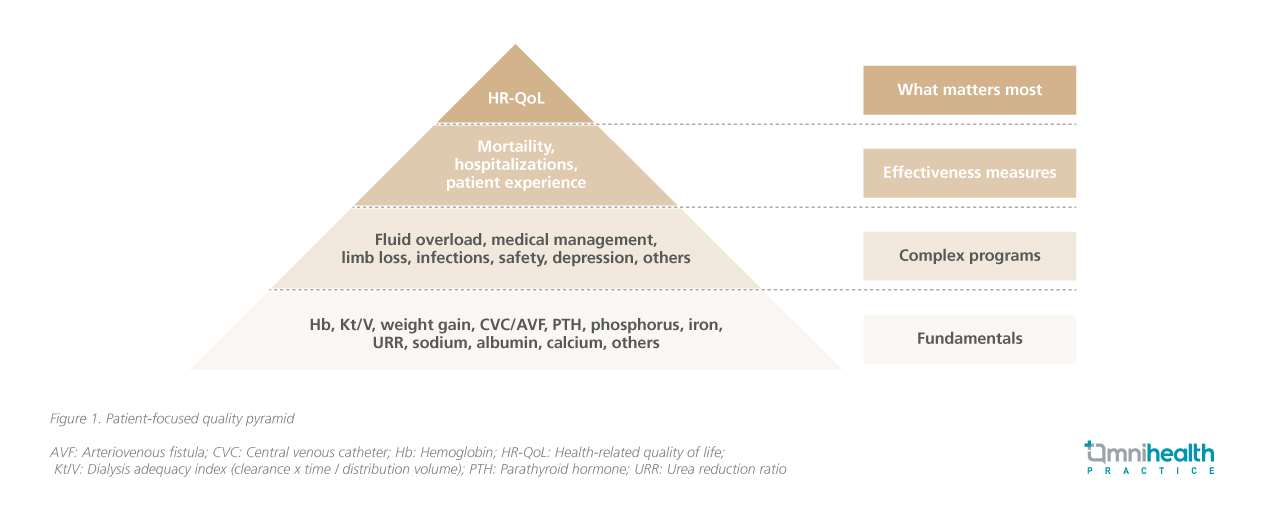
Dr. Fong later turned the spotlight toward how technological innovation could enable this transformation. The role of nephrologists is becoming more holistic, as ultimately, what matters most to patients is quality of life, not just survival on dialysis (figure 1).
Conventional hemodialysis (HD) uses a single-pass system, in which dialysate passes through the dialyzer once and is then discarded.7 While effective, Dr. Fong highlighted that this approach is resource-intensive, requiring large volumes of purified water and chemical concentrates. To improve efficiency, sorbent-based recirculating systems have been developed, which purify and regenerate dialysate, reducing both water and chemical consumption.8
The REDY (Recirculating Dialysate) system, introduced in the 1970s and now undergoing modern refinements, exemplifies sorbent-based dialysis, using compounds such as zirconium to remove uremic toxins from dialysate.8 Building on this concept, a new generation of compact devices has emerged.8 The NeoKidneyTM portable dialysis device, developed by Nextkidney, recently entered first-in-human trials and was presented at ASN Kidney Week 2024.9 Designed for home HD, it recycles a small volume of dialysate, drastically reducing water use and waste generation while giving patients greater independence.9 Similarly, AWAK (Automated Wearable Artificial Kidney), a Singapore-based peritoneal dialysis device, regenerates dialysate on-site using sorbent technology, although early trials reported challenges with abdominal discomfort.8 Other experimental systems include ViWAK, WEAKID, and CLS, are exploring wearable or miniaturized sorbent-based dialysis, emphasizing portability and environmental sustainability.8 Collectively, these innovations promise a paradigm shift toward dialysis that is not only more efficient but also more patient-centered, freeing individuals from the constraints of hospital-based treatment.8
The future horizon: toward miniaturization and functional restoration
Future artificial kidney development follows two major paths: miniaturization and restoration of native renal functions. Miniaturization is driving the creation of implantable devices, supported by advances in membrane engineering.8 These designs may allow more frequent and prolonged dialysis with less hemodynamic stress, potentially improving outcomes and reducing treatment burden.8 Implantable artificial kidneys (IAKs), combine silicon nanopore membranes with renal cell bioreactors, offer a promising platform for restoring metabolic and endocrine functions such as erythropoietin production and vitamin D activation.8 Preclinical efforts are now focused on achieving thrombosis resistance and biocompatibility, a critical yet aspirational requirements for a safe and long-term implantation.8
In parallel, biological approaches are also reshaping the vision of future kidney care. Dr. Fong highlighted biogenic kidneys from tissue engineering and 3D bioprinting with bioinks as regenerative strategies, while xenotransplantation using genetically engineered animal kidneys offers another potentially transformative path. He noted, “While many of these innovations are still years from clinical use, the trajectory toward a more personalized, less resource-intensive, and less hospital-dependent model is already taking shape.”
Conclusion
In conclusion, green nephrology is both an ethical responsibility and a frontier of innovation.6,8 The call to reduce environmental footprint of dialysis is no longer a distant ideal but a present mandate, and emerging technologies are bringing this goal closer within reach.3,8 By aligning green principles with technological advances, the kidney community can reimagine care that is not only life-saving but also life-sustaining for patients, health systems, and the planet.
References
- Sahani M, et al. Impacts of climate change and environmental degradation on children in Malaysia. Front Public Health. 2022;10:909779.
- Lenzen M, et al. The environmental footprint of health care: a global assessment. Lancet Planet Health. 2020;4(7):e271-9.
- Hoenich NA, et al. Clinical waste generation from renal units: implications and solutions. Sem Dial. 2005;18(5):396-400.
- Bharati J, et al. Environmental change and kidney health. Wits J Clin Med. 2022;4(3):141-9.
- Kidney disease: a global health priority. Nat Rev Nephrol. 2024;20(7):421-423.
- Sahay M, et al. Assessment of Biomedical Waste Generation in Dialysis Units: A Prospective Observational Study-Is it Time for “Green Dialysis”. J Assoc Physicians India. 2023;71(10):49-52.
- Selection and use of machine, dialyzer and dialysis fluid for maintenance hemodialysis. Indian J Nephrol. 2020;30(Suppl. 1):S9-S17.
- Tang YS, et al. Artificial kidney engineering: the development of dialysis membranes for blood purification. Membranes. 2022;12(2):177.
- Lau TW, et al. First-in-Human Trial of the NeoKidney Portable Hemodialysis Device Sorbent System: FR-OR23. J Am Soc Nephrol. 2024;35(10S):10-681.